Risk factors
Q. What is the most common bone site of osteomyelitis?
Osteomyelitis can be the result of a spreading infection in the blood (hematogenous) and occurs more often in children than adults. In prepubescent children, it usually affects the long bones: the tibia and the femur. The most common site of infection is the metaphysis, which is the narrow portion of the long bone).
Table of Contents
- Q. What is the most common bone site of osteomyelitis?
- Q. What does osteomyelitis look like?
- Q. What is the most common cause of osteomyelitis?
- Q. What does osteomyelitis pain feel like?
- Q. What happens if osteomyelitis is not treated?
- Q. How quickly does osteomyelitis spread?
- Q. What are the long term effects of osteomyelitis?
- Q. Is osteomyelitis an emergency?
- Q. What antibiotics are used to treat osteomyelitis?
- Q. Can osteomyelitis lay dormant?
- Q. Is osteomyelitis an autoimmune disease?
- Q. What is the treatment for chronic osteomyelitis?
- Q. Is Crmo a disability?
- Q. Can you have osteomyelitis without fever?
- Q. Is osteomyelitis very painful?
- Q. How do you know if you have a bone infection?
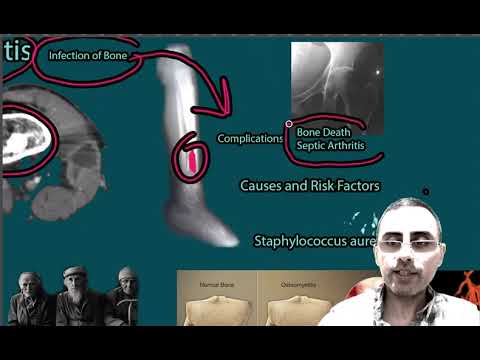
Q. What does osteomyelitis look like?
The features of acute osteomyelitis that may be visible include a periosteal reaction secondary to elevation of the periosteum (Figure 2), a well-circumscribed bony lucency representing an intraosseous abscess (Figure 3) and soft tissue swelling.
- Long term skin infections.
- Inadequately controlled diabetes.
- Poor blood circulation (arteriosclerosis).
- Risk factors for poor blood circulation, which include high blood pressure, cigarette smoking, high blood cholesterol and diabetes.
- Immune system deficiency.
- Prosthetic joints.
Q. What is the most common cause of osteomyelitis?
Most cases of osteomyelitis are caused by staphylococcus bacteria, types of germs commonly found on the skin or in the nose of even healthy individuals. Germs can enter a bone in a variety of ways, including: The bloodstream.
Q. What does osteomyelitis pain feel like?
Sometimes, bone lesions can cause pain in the affected area. This pain is usually described as dull or aching and may worsen during activity. The person may also experience fever and night sweats. In addition to pain, some cancerous bone lesions can cause stiffness, swelling, or tenderness in the affected area.
Q. What happens if osteomyelitis is not treated?
Osteomyelitis is a bacterial, or fungal, infection of the bone. Osteomyelitis affects about 2 out of every 10,000 people. If left untreated, the infection can become chronic and cause a loss of blood supply to the affected bone. When this happens, it can lead to the eventual death of the bone tissue.
Q. How quickly does osteomyelitis spread?
Acute osteomyelitis develops rapidly over a period of seven to 10 days.
Q. What are the long term effects of osteomyelitis?
Osteomyelitis needs long-term care to prevent complications such as: Fractures of the affected bone. Stunted growth in children, if the infection has involved the growth plate. Tissue death (gangrene) in the affected area.
Q. Is osteomyelitis an emergency?
Osteomyelitis can present to the emergency department as an acute, subacute, or chronic orthopedic concern.
Q. What antibiotics are used to treat osteomyelitis?
For osteomyelitis caused by anaerobic gram-negative bacteria, clindamycin, metronidazole, beta-lactam/beta lactamase inhibitor combinations, or carbapenems are the drugs of choice.
Q. Can osteomyelitis lay dormant?
However, for some people, osteomyelitis or septic arthritis may never completely go away. The bacteria can lie dormant in the body and return, even after treatment.
Q. Is osteomyelitis an autoimmune disease?
Involvement of the clavicle is the classical picture; however, the metaphyses and epiphyses of the femur, tibia or humerus are also frequently affected. Lesions may occur in any bone, including vertebrae [3, 4]. CRMO has recently been classified as an autoinflammatory disorder (rather than autoimmune).
Q. What is the treatment for chronic osteomyelitis?
Chronic osteomyelitis is generally treated with antibiotics and surgical debridement but can persist intermittently for years with frequent therapeutic failure or relapse. Despite advances in both antibiotic and surgical treatment, the long‐term recurrence rate remains around 20%.
Q. Is Crmo a disability?
Conclusion. In summary, CRMO is an autoinflammatory disease of the bone in children that can cause chronic debilitating pain and disability.
Q. Can you have osteomyelitis without fever?
People often do not have fever, which is usually the most obvious sign of an infection. Chronic osteomyelitis may develop if osteomyelitis is not treated successfully. It is a persistent infection that is very difficult to get rid of.
Q. Is osteomyelitis very painful?
Osteomyelitis is a painful bone infection. It usually goes away if treated early with antibiotics. If not, it can cause permanent damage.
Q. How do you know if you have a bone infection?
To diagnose a bone or joint infection, your doctor first performs a physical exam, looking for any open sores or areas of tenderness, swelling, and redness. He or she may ask if you’ve had any recent infections or surgery, of if you’ve experienced any pain or decreased range of motion in the affected limb or joint.