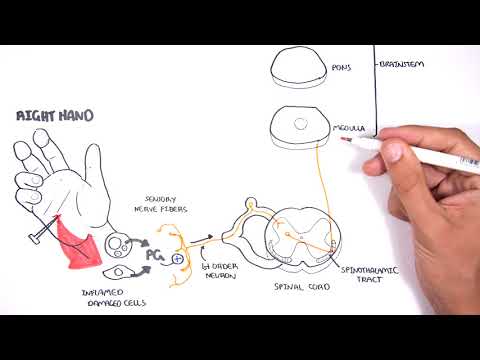
The medial thalamus projects to widespread areas of the forebrain, including the somatosensory cortex (Jones and Leavitt, 1974). Thus there are two major ascending pathways for pain: a direct lateral spinothalamic pathway and an indirect medial spinoreticulothalamic pathway.
Q. What does the descending pathway consist of?
Descending pathways are groups of myelinated nerve fibers that carry motor information from the brain or brainstem to effector’s muscles, via the spinal cord. They can be functionally divided into two groups: Pyramidal (voluntary) and extrapyramidal (involuntary) tracts.
Table of Contents
- Q. What does the descending pathway consist of?
- Q. What is descending pain pathway?
- Q. Where does the descending pain pathway originate?
- Q. What is the descending pain modulatory system?
- Q. What is descending modulation?
- Q. What is neurological pain?
- Q. What does neurological pain feel like?
- Q. What is the most reliable indicator of neurological status?
- Q. What is the first sign of a change in neurological status?
- Q. What is the most sensitive indicator of a brain injury?
- Q. What are the three types of TBI?
- Q. How is most traumatic brain injury diagnosed Currently scale?
Q. What is descending pain pathway?
Descending projections from the RVM extend to spinal cord dorsal horns where they connect to primary afferent terminals, second- and third-order neurons, as well as interneurons and thus inturn either inhibit or facilitate the pain sensation.
Q. Where does the descending pain pathway originate?
Originating in the brainstem, the descending noradrenergic pathways can be activated by EA manipulation through the DLF (Hu et al., 2016).
Q. What is the descending pain modulatory system?
Abstract. The descending pain modulatory system (DPMS) constitutes a network of widely distributed brain regions whose integrated function is essential for effective modulation of sensory input to the central nervous system and behavioural responses to pain.
Q. What is descending modulation?
Definition. Descending pain modulation encompasses pathways that descend from the forebrain and brainstem to the spinal cord and trigeminal sensory complex to modify incoming somatosensory information so that the perception of and reactions to somatosensory stimuli are altered, resulting in either less or more pain.
Q. What is neurological pain?
A neurological pain syndrome is chronic (long-term) pain that occurs when your nervous system does not work properly because of a disease or direct damage to a nerve or nerves. With some syndromes, the nerves signal pain even when there is not real feeling of pain.
Q. What does neurological pain feel like?
The pain is usually described as a burning sensation and affected areas are often sensitive to the touch. Symptoms of neuropathic pain may also include excruciating pain, pins and needles, difficulty correctly sensing temperatures and numbness.
Q. What is the most reliable indicator of neurological status?
The most accurate and reliable indicator of neurologic status is the level of consciousness. Pupillary evaluation is the second major component of the neurologic assessment.
Q. What is the first sign of a change in neurological status?
Symptoms of neurological changes often vary but can include sensory changes, motor changes, reflex changes, altered awareness and/or personality, altered level of consciousness and headaches (Koutoukidis et al.
Q. What is the most sensitive indicator of a brain injury?
The ASCOT probability of survival, which includes coded variables for the GCS, systolic blood pressure, and respiratory rates on admission, as well as a measure of multisystem anatomic injury, was the most sensitive indicator of head injury severity and was associated with outcomes beyond survival and death in this …
Q. What are the three types of TBI?
There are three basic levels of TBI injury: mild, moderate, and severe.
Q. How is most traumatic brain injury diagnosed Currently scale?
Computerized tomography (CT) scan. This test is usually the first performed in an emergency room for a suspected traumatic brain injury.