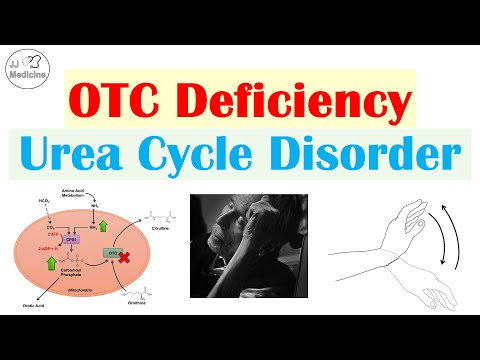
Ornithine transcarbamylase (OTC) deficiency is a rare X-linked genetic disorder characterized by complete or partial lack of the enzyme ornithine transcarbamylase (OTC). OTC is one of six enzymes that play a role in the break down and removal of nitrogen the body, a process known as the urea cycle.
Q. What is OTD disorder?
Ornithine transcarbamylase deficiency is an inherited disorder that causes ammonia to accumulate in the blood. Ammonia, which is formed when proteins are broken down in the body, is toxic if the levels become too high. The nervous system is especially sensitive to the effects of excess ammonia.
Table of Contents
- Q. What is OTD disorder?
- Q. What might cause the lack of N-Acetylglutamate?
- Q. What are the disorders of urea cycle?
- Q. What causes Citrullinemia?
- Q. Is Citrullinemia common?
- Q. What are the causes of hyperammonemia?
- Q. Why is arginine given in Citrullinemia?
- Q. What is Arginosuccinase aciduria?
- Q. What are normal citrulline levels?
- Q. What is Argininosuccinate lyase deficiency?
- Q. What is the cause of Argininosuccinate lyase deficiency?
- Q. What type of enzyme is Argininosuccinase?
- Q. What is ASL gene?
- Q. Is Argininosuccinate used to build proteins?
- Q. Is cleaved by argininosuccinate lyase to arginine and fumarate?
- Q. Which gene makes an enzyme that is responsible for directly producing arginine succinate?
- Q. What enzyme converts citrulline to Argininosuccinate?
- Q. Is Argininemia dominant or recessive?
- Q. What is arginine genetics?
- Q. What are the symptoms of arginine deficiency?
- Q. When should you take L-Arginine?
- Q. Why the absence of arginine can lead to ammonia toxicity?
- Q. What hereditary condition arginine becomes essential?
- Q. Why arginine is given in hyperammonemia?
- Q. How common is arginase deficiency?
Q. What might cause the lack of N-Acetylglutamate?
NAGS deficiency is an autosomal recessive genetic disorder caused by mutations of the NAGS gene. Mutations in the NAGS gene results in deficiency of the enzyme N-acetylglutamate synthetase. The symptoms of NAGS deficiency develop due to the lack of this enzyme which is needed to break down nitrogen in the body.
Q. What are the disorders of urea cycle?
A urea cycle disorder (UCD) is an inherited disease that affects how the body removes the waste that is made from breaking down protein. Everyone needs protein, which is found in foods like dairy products, meat and fish.
Q. What causes Citrullinemia?
As ammonia builds up, muscle weakness, seizures , coma, and death can occur. Citrullinemia is caused by mutations in the ASS1 gene and is inherited in an autosomal recessive pattern. This disorder is diagnosed through newborn screening and additional medical and genetic tests.
Q. Is Citrullinemia common?
Frequency. Type I citrullinemia is the most common form of the disorder, affecting about 1 in 57,000 people worldwide. Type II citrullinemia is found primarily in the Japanese population, where it occurs in an estimated 1 in 100,000 to 230,000 individuals.
Q. What are the causes of hyperammonemia?
Acquired hyperammonemia is usually caused by diseases that result in either acute liver failure, such as overwhelming hepatitis B or exposure to hepatotoxins, or cirrhosis of the liver with chronic liver failure. Chronic hepatitis B, chronic hepatitis C, and excessive alcohol consumption are common causes of cirrhosis.
Q. Why is arginine given in Citrullinemia?
Arginine, sodium benzoate and sodium phenylacetate help to remove ammonia from the blood. Dialysis may be used to remove ammonia from the blood when it reaches critical levels.
Q. What is Arginosuccinase aciduria?
Argininosuccinic aciduria – also known as argininosuccinase deficiency and argininocuccinate lyase deficiency (ALD) – is an inherited disorder that causes ammonia to accumulate in the blood. Ammonia is toxic if the levels become too high.
Q. What are normal citrulline levels?
Amino acid levels and ARDS The median plasma level of citrulline was very low at 9.2 uM (interquartile range (IQR) 5.2 to 14.4) compared to a normal range of 40 ± 10 uM in healthy adults [16]. The median plasma level of arginine was also low at 22.7 uM (IQR 12.8 to 37.9) compared to a normal range of 27 to 80 uM.
Q. What is Argininosuccinate lyase deficiency?
Defect: Argininosuccinate Lyase (ASL) Deficiency, also known as Argininosuccinic Aciduria (AA), is the result of a mutated or deficient argininosuccinate lyase enzyme. This defective or deficient enzyme leads to inadequate ureagenesis, accumulation of argininosuccinic acid, and deficient endogenous arginine production.
Q. What is the cause of Argininosuccinate lyase deficiency?
Alterations in the ASL gene lead to low levels of functional argininosuccinate lyase, which is needed to break down nitrogen in the body. Failure to properly break down nitrogen leads to the abnormal accumulation of nitrogen, in the form of ammonia, in the blood (hyperammonemia).
Q. What type of enzyme is Argininosuccinase?
ASL (argininosuccinate lyase, also known as argininosuccinase) is an enzyme that catalyzes the reversible breakdown of argininosuccinate (ASA) producing the amino acid arginine and dicarboxylic acid fumarate.
Q. What is ASL gene?
The ASL gene encodes the subunit of argininosuccinate lyase (EC 4.3. 2.1) is a urea cycle enzyme that catalyzes the cleavage of argininosuccinate to fumarate and arginine, an essential step in the process of detoxification of ammonia via the urea cycle (O’Brien et al., 1986).
Q. Is Argininosuccinate used to build proteins?
The specific role of the argininosuccinate lyase enzyme is to start the reaction in which the amino acid arginine, a building block of proteins, is produced from argininosuccinate, the molecule that carries the waste nitrogen collected earlier in the urea cycle.
Q. Is cleaved by argininosuccinate lyase to arginine and fumarate?
5 Argininosuccinic Aciduria. ASA is cleaved into two smaller molecules, arginine and fumarate, in an equilibrium reaction catalyzed by ASA lyase. The enzyme is active in the liver, brain, and kidney. The enzyme is also measurable in the red blood cells and fibroblasts.
Q. Which gene makes an enzyme that is responsible for directly producing arginine succinate?
Argininosuccinate lyase (ASL) is the enzyme that catalyzes the fourth step in the urea cycle, in which argininosuccinic acid is cleaved to produce arginine and fumarate.
Q. What enzyme converts citrulline to Argininosuccinate?
Argininosuccinate synthase
Q. Is Argininemia dominant or recessive?
Argininemia has an autosomal recessive pattern of inheritance.
Q. What is arginine genetics?
Arginase deficiency is an inherited disorder that causes the amino acid arginine (a building block of proteins) and ammonia to accumulate gradually in the blood. Ammonia, which is formed when proteins are broken down in the body, is toxic if levels become too high.
Q. What are the symptoms of arginine deficiency?
Symptoms
- Poor growth (present in all the people who have arginase deficiency)
- Stiff muscles and increased reflexes ( spasticity )
- Developmental delay.
- Loss of previously acquired developmental milestones.
- Intellectual disability.
- Seizures.
- Small head size ( microcephaly )
- Problems with balance and coordination.
Q. When should you take L-Arginine?
Taking L-arginine L-arginine should be taken at least 3 times a day: in the morning and one each before and after working out. The recommended dose is between 2 to 6 grams. This can be taken before working out to increase blood flow, thus increasing your energy.
Q. Why the absence of arginine can lead to ammonia toxicity?
(b) Oxidative deamination of amino acids caused the elevation of ammonia levels. In addition, the lack of arginine (an intermediate in the urea cycle) slowed the conversion of ammonia to urea. (c) Ornithine (or citrulline) can be substituted for arginine because it also is an intermediate in the urea cycle.
Q. What hereditary condition arginine becomes essential?
Arginine becomes essential under conditions of stress and catabolic states when capacity of endogenous arginine synthesis is surpassed, including hemolytic anemias,891011–12 asthma,1314–15 pregnancy, and critical illness such as sepsis, burns, and trauma.
Q. Why arginine is given in hyperammonemia?
l-arginine increases ammonia elimination by increasing l-citrulline and argininosuccinate production [29,30]. l-citrulline administration restores l-arginine levels in N-acetylglutamate synthetase and carbamoyl phosphate synthetase-1 deficiencies and supports the urea cycle [30].
Q. How common is arginase deficiency?
Arginase-1 deficiency has been estimated to occur in approximately 1 in 300,000-1,000,000 births. Arginase-1 deficiency is among the least common of all the disorders of the urea cycle.