Q. What is secondary follicle?
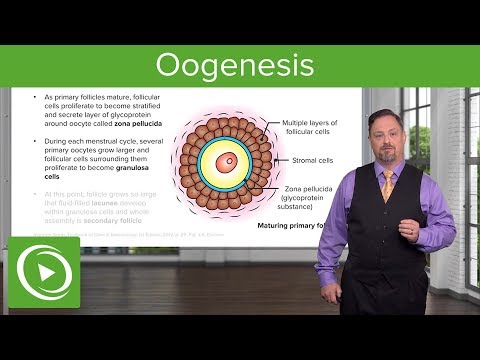
A secondary ovarian follicle is a maturing ovarian follicle consisting of an oocyte surrounded by two or more layers of tall, supporting granulosa cells.
Q. What are the stages of follicular developments?
Preantral follicular development can be divided into three stages: activation of primordial follicles, the primary to secondary follicle transition, and the development of secondary follicles to the periantral stage.
Table of Contents
- Q. What is secondary follicle?
- Q. What are the stages of follicular developments?
- Q. What does a secondary follicle turn into?
- Q. What is the difference between a primary and secondary follicle?
- Q. At what point does a primary follicle become a secondary follicle in a female?
- Q. What is the difference between secondary follicle and tertiary follicle?
- Q. What hormone does the secondary follicle produce?
- Q. What is meant by tertiary follicle?
- Q. What is the final stage in the process of ovarian follicle development?
- Q. Can follicles grow in 2 days?
- Q. What are the two stages of follicle recruitment?
- Q. What is the best size of follicle to conceive?
- Q. What is the normal size of follicle to rupture?
- Q. Is 24mm follicle too big?
- Q. Can a 14mm follicle release an eggs?
- Q. Can I get pregnant with 20 mm follicle?
- Q. Is a 21mm follicle good?
- Q. Can you get pregnant with 2 follicles?
- Q. Can you get pregnant with only one mature follicle?
Q. What does a secondary follicle turn into?
The secondary follicle develops into a Graffian follicle. The oocyte, zona pellucida and the follicular cells surrounding the ooctye (known as the corona radiata) are all expelled at ovulation, and enter the fallopian tube. Once released, the oocyte begins its second meiotic division, as far as metaphase II.
Q. What is the difference between a primary and secondary follicle?
A primary follicle is an immatured ovarian follicle surrounded by single layer of cuboidal cells. They are known as granulosa cells. Secondary follicles consists of many layers of cuboidal cells known as membrana granulosa cells.It secreates follicular fluid.
Q. At what point does a primary follicle become a secondary follicle in a female?
Until the preovulatory stage, the follicle contains a primary oocyte that is arrested in prophase of meiosis I. During the late preovulatory stage, the oocyte continues meiosis and becomes a secondary oocyte, arrested in metaphase II.
Q. What is the difference between secondary follicle and tertiary follicle?
A secondary follicle is formed from the primary follicle as it gets surrounded by more layers of granulosa cells and a theca layer is formed outside the basal lamina. The tertiary follicle is characterised by the formation of antrum, which is a fluid-filled cavity.
Q. What hormone does the secondary follicle produce?
The follicles also release a second hormone called inhibin, which also suppresses further production of FHS. As the oestrogen levels rise, this triggers a a mid cycle surge in a second pituitary hormone called Lutenising hormone (LH), which causes the follicle to rupture (ovulation).
Q. What is meant by tertiary follicle?
n. A cavity in the ovary containing a maturing ovum surrounded by its encasing cells. Link to this page: ovarian follicle
Q. What is the final stage in the process of ovarian follicle development?
Select antral follicles are rescued from atresia by responding to the cyclic changes in FSH secretion, and they become preovulatory follicles that are capable of oocyte release and corpora lutea formation. This final stage of development is gonadotropin-dependent and is known as cyclic recruitment.
Q. Can follicles grow in 2 days?
Currently, transvaginal ultrasound is used to monitor the follicular growth by simply measuring the follicles. Follicles grow approximately 2 mms per day so there is some predictability of when the follicles will reach the appropriate size for ovulation or retrieval.
Q. What are the two stages of follicle recruitment?
The follicles develop through primordial, primary, and secondary stages before acquiring an antral cavity. At the antral stage, most follicles undergo atretic degeneration, whereas a few of them, under the cyclic gonadotropin stimulation that occurs after puberty, reach the preovulatory stage (1, 2).
Q. What is the best size of follicle to conceive?
When your follicles have reached around 18-20mm in diameter they are deemed ready for egg collection. You’ll be given a hormone trigger injection to stimulate your follicles to release the mature eggs that have been prepared in your follicles.
Q. What is the normal size of follicle to rupture?
At the time of follicle rupture, the follicle should be preferably 18 mm or more in size and the endometrium should be at least 7 mm thick. A very thin lining cannot sustain pregnancy. What do I expect during follicular monitoring? Your gynaecologist would call you for ultrasound on days 2, 9, 11, 13, 14, 15 (roughly).
Q. Is 24mm follicle too big?
Usually once the follicle is greater than 24 mms, the egg within is overmature and therefore no longer viable. Ovulation may occur but that is the main problem.
Q. Can a 14mm follicle release an eggs?
Smaller follicles 10-14 mm usually do not give us an egg, and if they do, the egg is most often immature. In addition, many of the follicles in women over 40 or those with DOR, are empty since the eggs may have degenerated over time.
Q. Can I get pregnant with 20 mm follicle?
Results: Data from 516 IUI cycles were analyzed. Frequencies of clinical pregnancy, ongoing pregnancy, and live birth for a follicle size of 19-20 mm were 30.2% (39/129), 24.0% (31/129), and 24.0% (31/129), respectively; these rates were significantly higher than those in other groups (all P<0.05).
Q. Is a 21mm follicle good?
The follicle size is appropriate for the stage of your cycle and ovulation should occur quite likely on day 13 or 14. The follicles usually start at 5-6mm and progressively increase until about 20-21mm before the egg is released.
Q. Can you get pregnant with 2 follicles?
Every mature sized follicle could release an egg, and that egg could become fertilized. If you have two follicles, you could conceive twins.
Q. Can you get pregnant with only one mature follicle?
Each follicle contains just one egg, but it takes just one egg to get pregnant. For the best possible chance of a successful conception and pregnancy, optimum health of the egg and sperm is imperative. Impryl is a dietary supplement that contains the essential micronutrients needed to optimise sperm or egg quality.