Thick and thin blood smears. These are the most common and accurate malaria tests. A lab technician, doctor, or nurse will take some of your blood and send it to a lab to be stained to make any parasites show clearly.
Q. Why is fixing the smear important?
The preparation of a smear is required for many laboratory procedures, including the Gram-stain. The purpose of making a smear is to fix the bacteria onto the slide and to prevent the sample from being lost during a staining procedure. A smear can be prepared from a solid or broth medium.
Table of Contents
- Q. Why is fixing the smear important?
- Q. Why are smears for capsule staining not fixed by heat?
- Q. What is the disadvantage of having a really thick smear when staining?
- Q. What are the stages of malaria parasite?
- Q. Which test should be done for malaria?
- Q. What if malaria test is negative?
- Q. What is the gold standard for malaria diagnosis?
- Q. How do I read a malaria test report?
- Q. What is the normal range of malaria?
- Q. When should malaria test be done?
- Q. Can malaria be cured by antibiotics?
- Q. What are side effects of chloroquine?
- Q. Is chloroquine a steroid?
- Q. Does chloroquine affect the brain?
- Q. Can chloroquine cause blindness?
- Q. How is chloroquine poisoning treated?
- Q. Can hydroxychloroquine cause liver damage?
- Q. What are the symptoms of a hydroxychloroquine overdose?
- Q. How much hydroxychloroquine is lethal?
Q. Why are smears for capsule staining not fixed by heat?
Most bacterial capsules are composed of polysaccharide however some genera produce polypeptide capsules. Capsular material is very moist (slimy) and any heating will cause it to shrink – it is for this reason that we will not heat fix the slide before staining.
Q. What is the disadvantage of having a really thick smear when staining?
Do NOT make your smear suspensions too thick. The dye will not penetrate well, and there will be far too many bacterial cells to see individual shapes and arrangements. One needs to be careful about thick smears when taking the specimen from an agar medium.
Q. What are the stages of malaria parasite?
The malaria parasite life cycle involves two hosts. During a blood meal, a malaria-infected female Anopheles mosquito inoculates sporozoites into the human host . Sporozoites infect liver cells and mature into schizonts , which rupture and release merozoites .
Q. Which test should be done for malaria?
PCR is most useful for confirming the species of malarial parasite after the diagnosis has been established by either smear microscopy or RDT. Serology detects antibodies against malaria parasites, using either indirect immunofluorescence (IFA) or enzyme-linked immunosorbent assay (ELISA).
Q. What if malaria test is negative?
A normal test is negative, meaning that you don’t have any Plasmodium parasites in your blood. A positive result means that you have the parasites in your blood and that you may have malaria.
Q. What is the gold standard for malaria diagnosis?
The gold standard for the diagnosis of malaria involves microscopy with visualization of Giemsa-stained parasites in a blood sample. Species determination is made based on morphological characteristics of the four species of human malaria parasites and the infected red blood cells.
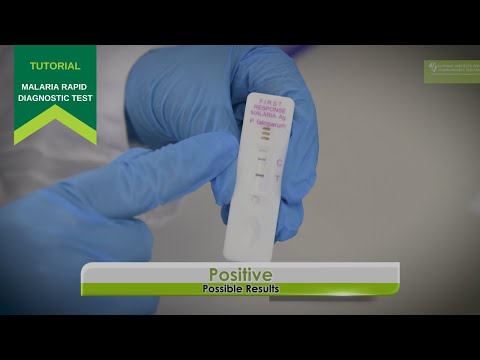
Q. How do I read a malaria test report?
- A line near letter “C” followed by one or two lines near letter “t” means the patient is positive for malaria as shown below. (Test is positive even if the test lines are faint.)
- 2.Put on the gloves.
- for each patient.
- Check the expiry date on the test.
- packet.
- Open the packet and remove: 4.
- a.
- Open the alcohol swab.
Q. What is the normal range of malaria?
The threshold of detection by these rapid diagnostic tests is in the range of 100 parasites/µl of blood (commercial kits can range from about 0.002% to 0.1% parasitemia) compared to 5 by thick film microscopy.
Q. When should malaria test be done?
Why do I need a malaria test? You may need this test if you live or have recently traveled to an area where malaria is common and you have symptoms of malaria. Most people will have symptoms within 14 days of being bitten by an infected mosquito.
Q. Can malaria be cured by antibiotics?
To overcome this problem new therapeutic strategies are been developed. Many other drugs formulations have recently been developed such as combination of molecules (artemisinin-based combination therapy) [4] and use of antibiotics that have been shown to be effective against malaria parasites [5, 6].
Q. What are side effects of chloroquine?
Side effects from chloroquine phosphate can occur. Tell your doctor if any of these symptoms are severe or do not go away:
- headache.
- nausea.
- loss of appetite.
- diarrhea.
- upset stomach.
- stomach pain.
- rash.
- itching.
Q. Is chloroquine a steroid?
Steroid-sparing treatments have been sought and one of these is chloroquine. Chloroquine is an anti-inflammatory agent, also used in the treatment of malarial infection and as a second-line therapy in the treatment of rheumatoid arthritis, sarcoidosis and systemic lupus erythematosus.
Q. Does chloroquine affect the brain?
Discussion: Chloroquine may achieve high concentrations in the brain and has a long half-life. As quinolines, the antimalarials may have the same pathologic activity as the fluoroquinolone antibiotics in acting as N-methyl-d-aspartate agonists and gamma-aminobutyric acid antagonists.
Q. Can chloroquine cause blindness?
Blindness from Chloroquine is irreversible and unfortunately visual loss will progress despite cessation of therapy. Three patients with retinopathy are told to stop using chloroquine and use alternative antimalarials. Most of these patients with low vision will benefit from low vision aids.
Q. How is chloroquine poisoning treated?
These preliminary data suggest that combining early mechanical ventilation with the administration of diazepam and epinephrine may be effective in the treatment of severe chloroquine poisoning.
Q. Can hydroxychloroquine cause liver damage?
Mechanism of Injury. Hydroxychloroquine is metabolized in the liver and may alter metabolism of other medications. Therapy is unlikely to cause liver injury in normal individuals, but can trigger an acute worsening of porphyria cutanea tarda in susceptible individuals.
Q. What are the symptoms of a hydroxychloroquine overdose?
An overdose of hydroxychloroquine can be fatal, and must be treated quickly. Overdose symptoms may include drowsiness, vision changes, seizure, slow heart rate, weak pulse, pounding heartbeats, sudden dizziness, fainting, shortness of breath, or slow breathing (breathing may stop).
Q. How much hydroxychloroquine is lethal?
The lethal dose of the drug is not well established, although severe symptoms occur with ingestion of 4 gm, and fatalities have been associated with ingestion of 12 gm. The utility and accuracy of serum hydroxychloroquine levels for prognostication and management is an important question.